The NHS in 2026: From rhetoric to reality
UK health policy and market outlook
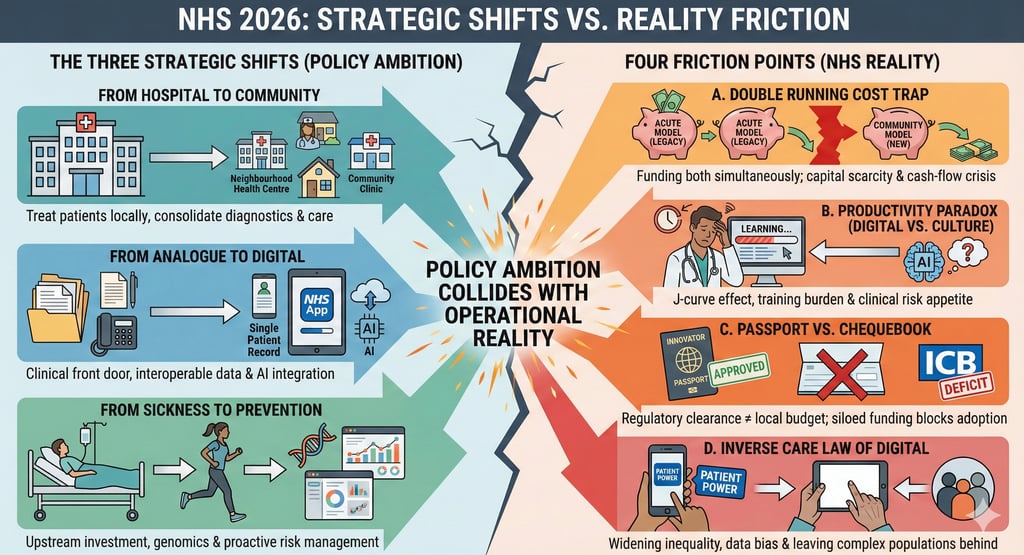
If 2025 was the year of diagnosis, marked by the publication of the 10-Year Health Plan, the Life Sciences Sector Plan, Medium Term Planning Framework, and the NICE forward view, 2026 is the year of surgery. The rhetoric of "fundamental reinvention" is now hitting the operational reality of the NHS.
For stakeholders across the ecosystem, the "wait and see" period is over. The direction of travel is locked in: a decisive move away from acute-centric, analogue sick care toward a preventative, community-based, digital-first health system.
The strategic context: Three shifts
The NHS care model is being re-engineered around three specific shifts. In 2026, these move from high-level ambitions to contractual requirements:
From hospital to community: The goal is to treat patients in "Neighbourhood Health Centres" that consolidate diagnostics, post-operative care, and primary care, reducing acute hospital footfall.
From analogue to digital: Transitioning the NHS App from a booking tool to a clinical "front door," supported by a Single Patient Record
From sickness to prevention: Moving budget upstream into genomics and population health management to intercept disease before it requires acute intervention.
The "10-Year Health Plan" has moved the NHS into a phase of hard pencils and difficult choices.
For the industry, the market is becoming both more centralised (via the Innovator Passport if and when it lands and ICB consolidation) and more decentralised with more power and freedom for (some) Trusts. Overall, the health system is more demanding regarding value.
In 2026, the NHS is open for business, but only for those who can prove they keep patients at home, data flowing, and costs down. The NHS 10 Year Plan, Medium Term Framework and NICE’s priorities made it clear what the health service is looking for from industry.
Moving beyond the press releases
Why the 2026 Vision might stall, and where the real opportunities lie.
While the 10-Year Plan provides the roadmap, the terrain is difficult. I see four specific friction points where policy ambition collides with NHS reality. Understanding these is crucial for your strategy.
A. The "double running" cost trap
The theory: Shifting care from hospitals to the community reduces expensive acute activity, freeing up cash to reinvest in prevention.
The critical reality:
The transition gap: You cannot close a hospital ward the day you open a community clinic. There is a lag, likely months or even years, where the system must fund both the old acute model and the new community model simultaneously.
Capital scarcity: The NHS has a multi-billion pound maintenance backlog. Building or retrofitting "Neighbourhood Health Centres" requires capital that is historically scarce.
Risk for industry: If the Treasury does not fund this transition explicitly, ICBs will be forced to raid their transformation budgets just to keep the lights on. "Spend to save" projects (like your MedTech solution) might be paused due to cash-flow crises, even if the long-term ROI is proven.
B. The productivity paradox (digital vs. culture)
The theory: AI and digital tools will "liberate" staff time, delivering a 2% productivity gain.
The critical reality:
The "J-curve" effect: Digital transformation almost always lowers productivity before raising it. Staff need time to learn new systems (e.g., the Single Patient Record). In a system running at 99% capacity, there is no headroom for the learning curve.
Cultural inertia: An "AI Scribe" is useless if the consultant doesn't trust the output and spends 10 minutes checking the notes anyway. The barrier isn't the technology; it's the clinical risk appetite.
Implication: Tech vendors cannot just sell software; they must sell change management. Your implementation support team will be more valuable than your sales team in 2026.
C. The "passport" vs. the "chequebook"
The theory: The Innovator Passport and integrated MHRA/NICE pathway will smooth market access.
The critical reality:
Regulatory approval ≠ purchase order: A device might get a "Passport" (regulatory and clinical clearance), but if the local ICB is in a financial deficit, the answer is still "no."
Siloed budgets: Value-Based Procurement often fails because of the ‘wrong pocket problem’, where the cost falls on one budget (e.g., primary care) while the savings accrue in another (e.g., hospital, reduced bed days).
Advice: Don't rely solely on the Passport (if and when it lands). You still need a localised business case that speaks to the specific financial pain points of the ICB you are targeting.
D. The inverse care law of digital
The theory: The NHS App and "Patient Power" will equalise care.
The critical reality:
Widening the gap: Heavy reliance on the NHS App risks prioritising the "worried well" and the digital literates, who are typically younger, wealthier, and healthier. The complex, multi-morbid elderly population (who consume 70% of resources) may be left behind if the "analogue" routes are degraded too quickly.
Data bias: If AI models are trained primarily on data from digitally engaged patients, the algorithms may develop biases, leading to "precision medicine" that works best for a narrow, non-representative patient cohorts.
Opportunity: There is a massive, under-served market for "inclusive tech", solutions specifically designed for low-digital-literacy populations (e.g., voice-activated interfaces, non-smartphone remote monitoring).
So, what do I think? Cautious optimism
Is this time different? It might be. The difference in 2026 is the existential nature of the crisis. In previous years (e.g., the 2014 Five Year Forward View), reform was desirable; now, it is mandatory for survival.
For the health ecosystem players, the the change is coming:
Industry: Stop selling features; start selling capacity. If you can prove measurable impact on capacity, productivity, and enable the workforce, you can still win.
Providers: The era of the "fortress hospital" is over. Survival depends on integration with the community.
Payers: The courage to move money from acute to community (despite the headlines) will define the success of this generation of leaders.
2026 will be messy, unequal, and financially painful, but the alternative is systemic failure.